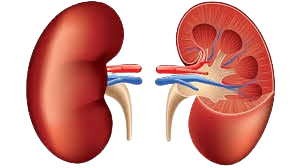
Nephrology (Kidney Speciality)
- Home
- Nephrology (Kidney Speciality)
Nephrology (Kidney Speciality)
Nephrology is a medical specialty that focuses on the diagnosis and treatment of kidney diseases, including chronic kidney disease, hypertension, and electrolyte imbalance. In India, nephrology departments provide advanced care such as dialysis, kidney transplantation, and management of kidney-related conditions. These departments benefit patients by providing specialized treatments, improving quality of life, and offering comprehensive management of kidney health. Medkins Healthcare helps you find the best renal care department in India, guiding you to top specialists and hospitals in your requested location and providing ongoing support throughout your treatment.
Diseases Treated by nephrology alone or with urology
Chronic Kidney Disease (CKD): A long-term condition where the kidneys gradually lose function over time. It is often caused by high blood pressure, diabetes, or glomerulonephritis.
Acute Kidney Injury (AKI): A sudden loss of kidney function, typically caused by dehydration, infections, drug toxicity, or blockage of the urinary tract. AKI is usually reversible if treated promptly.
Glomerulonephritis: Inflammation of the glomeruli, which are the tiny filtering units in the kidneys. This condition can result from infections, autoimmune diseases, or other causes, and may lead to kidney damage.
Polycystic Kidney Disease (PKD): A genetic disorder where fluid-filled cysts develop in the kidneys, causing them to enlarge and impair their function. This can lead to kidney failure over time.
Nephrotic Syndrome: A kidney disorder characterized by high levels of protein in the urine, low levels of protein in the blood, swelling, and high cholesterol levels. It is caused by damage to the glomeruli.
Diabetic Nephropathy: Kidney damage resulting from diabetes, where high blood sugar levels cause progressive damage to the kidneys’ filtering system, leading to CKD.
Hypertensive Nephropathy: Kidney damage caused by chronic high blood pressure, which leads to scarring and eventual kidney failure if untreated.
Kidney Stones (Nephrolithiasis): Solid masses made of crystals that develop in the kidneys and can cause severe pain when passing through the urinary tract. They can be caused by dehydration, high calcium levels, or other metabolic factors.
Renal Artery Stenosis: Narrowing of the arteries that supply blood to the kidneys, usually due to atherosclerosis. This can lead to high blood pressure and reduced kidney function.
Lupus Nephritis: An autoimmune condition where lupus causes inflammation and damage to the kidneys. It is a complication of systemic lupus erythematosus (SLE).
IgA Nephropathy (Berger’s Disease): A kidney disease caused by the buildup of immunoglobulin A (IgA) in the kidneys, leading to inflammation and damage to the kidney tissues.
Focal Segmental Glomerulosclerosis (FSGS): A type of glomerular disease where scar tissue forms in the kidneys, leading to nephrotic syndrome and eventually kidney failure.
Interstitial Nephritis: Inflammation of the kidney’s tubules and the spaces between them. This condition can result from infections, medications, or autoimmune disorders and can lead to AKI or CKD.
Alport Syndrome: A genetic disorder that affects the kidneys, ears, and eyes. It leads to progressive kidney disease, hearing loss, and vision problems due to abnormalities in the basement membrane of these organs.
Amyloidosis: A condition in which abnormal proteins called amyloids build up in the kidneys and other organs, leading to kidney dysfunction and, eventually, kidney failure.
Goodpasture Syndrome: A rare autoimmune disease where antibodies attack the kidneys and lungs, leading to rapidly progressive kidney failure and lung hemorrhage.
Fabry Disease: A genetic disorder that affects the kidneys and other organs due to the buildup of a fatty substance called globotriaosylceramide, which leads to kidney dysfunction and failure.
Renal Cell Carcinoma: A type of kidney cancer that originates in the lining of the renal tubules. It can cause symptoms like blood in the urine, flank pain, and weight loss.
Hydronephrosis: Swelling of one or both kidneys due to the buildup of urine. It occurs when there is a blockage or obstruction in the urinary tract, preventing urine from draining properly.
Renal Tubular Acidosis (RTA): A condition where the kidneys fail to properly acidify the urine, leading to an acid-base imbalance in the body. It can be hereditary or acquired.
Hemolytic Uremic Syndrome (HUS): A condition often triggered by infection, where red blood cells are destroyed and block the kidney’s filtering system, leading to AKI and other complications.
Minimal Change Disease: A disorder that affects the kidneys’ filtering ability, often seen in children, where the glomeruli appear normal under a microscope but cause nephrotic syndrome.
Conditions Treated by Nephrology alone or with Urology
Proteinuria: The presence of excess protein in the urine, often indicating kidney damage or disease, such as glomerulonephritis or nephrotic syndrome.
Hematuria: Blood in the urine, which can be caused by kidney stones, infections, trauma, or kidney disease like glomerulonephritis.
Electrolyte Imbalance: Abnormal levels of electrolytes such as sodium, potassium, and calcium, often resulting from kidney dysfunction, dehydration, or certain medications.
Acid-Base Disorders: Imbalance in the pH levels of the body, commonly seen in kidney disease. Examples include metabolic acidosis and metabolic alkalosis.
Hyperkalemia: Elevated potassium levels in the blood, often a result of kidney failure, as the kidneys cannot properly excrete potassium.
Hyponatremia: Low sodium levels in the blood, which can occur due to excessive fluid retention in kidney disease or other systemic conditions.
Fluid Overload: A condition where the body retains excessive fluid due to reduced kidney function, leading to swelling (edema), high blood pressure, and congestive heart failure.
Renal Hypertension: High blood pressure caused by kidney disease, particularly conditions like renal artery stenosis or chronic kidney disease.
Urinary Tract Obstruction: Blockage in the urinary tract (such as by kidney stones, tumors, or an enlarged prostate), which can lead to hydronephrosis, kidney damage, or infections.
Nephrogenic Diabetes Insipidus: A condition where the kidneys are unable to concentrate urine, leading to excessive thirst and urination, caused by damage to the kidneys or certain medications.
Acute Tubular Necrosis (ATN): A condition where kidney tubule cells are damaged due to lack of oxygen or toxins, leading to AKI and potentially kidney failure.
Oliguria/Anuria: Oliguria refers to reduced urine output, while anuria is the absence of urine production, often seen in severe kidney damage or obstruction.
Uremia: A condition where waste products that the kidneys normally remove build up in the blood, leading to symptoms like nausea, fatigue, confusion, and in severe cases, coma.
Anemia of Chronic Kidney Disease: A common complication of CKD where the kidneys fail to produce enough erythropoietin, a hormone that stimulates red blood cell production, leading to anemia.
Renal Osteodystrophy: A bone disorder that occurs when the kidneys fail to maintain proper levels of calcium and phosphorus, often seen in chronic kidney disease.
Dialysis-related Complications: Conditions such as low blood pressure, electrolyte imbalances, and infections that can occur in patients undergoing hemodialysis or peritoneal dialysis.
Procedures performed by Nephrology alone or with Urology
Hemodialysis: A life-saving procedure used to filter waste, toxins, and excess fluids from the blood when the kidneys are no longer able to function properly. Hemodialysis involves the use of a dialysis machine and a dialyzer (artificial kidney). It is typically performed in a hospital, clinic, or dialysis center.
Peritoneal Dialysis: A dialysis treatment that uses the lining of the abdomen (peritoneum) to filter blood inside the body. A special fluid (dialysate) is introduced into the abdominal cavity, which absorbs waste products and is then drained. It can be done at home, making it a more flexible option for some patients.
Kidney Biopsy (Renal Biopsy): A diagnostic procedure where a small piece of kidney tissue is removed and examined under a microscope. It is used to diagnose kidney disease, assess the severity of damage, and guide treatment decisions. It is performed using a needle guided by ultrasound or CT scan.
Arteriovenous (AV) Fistula Creation: A surgical procedure to create a connection between an artery and a vein, usually in the arm. This connection is used for long-term access to perform hemodialysis. An AV fistula provides a high blood flow that is ideal for dialysis.
Arteriovenous (AV) Graft: Similar to an AV fistula, but instead of connecting an artery and a vein directly, a synthetic tube (graft) is used. This is often performed when a patient’s veins are not suitable for creating a fistula.
Central Venous Catheter Placement (for Dialysis): A temporary procedure where a catheter is inserted into a large vein in the neck, chest, or groin for immediate access to the bloodstream for dialysis. This is often used in emergency situations or when long-term access has not yet been established.
Continuous Renal Replacement Therapy (CRRT): A type of dialysis used for critically ill patients in intensive care units (ICUs) who cannot tolerate standard hemodialysis. CRRT is performed continuously over 24 hours, allowing for gentler fluid and waste removal.
Plasma Exchange (Plasmapheresis): A procedure in which the plasma (the liquid part of the blood) is removed, filtered, and replaced with fresh plasma or a plasma substitute. This is used to treat autoimmune diseases, such as Goodpasture syndrome or vasculitis, where harmful antibodies in the plasma are attacking the kidneys.
Placement of Peritoneal Dialysis Catheter: A procedure to place a catheter in the abdomen for patients who will undergo peritoneal dialysis. The catheter allows for the introduction and drainage of the dialysate fluid used in the dialysis process.
Kidney Transplantation (in collaboration with Urology): A surgical procedure where a healthy kidney from a living or deceased donor is transplanted into a patient with end-stage renal disease (ESRD). Nephrologists manage the patient’s medical care before and after the transplant, including immunosuppressive therapy to prevent organ rejection.
Ultrasonography of the Kidneys: A non-invasive imaging procedure using ultrasound to assess kidney size, structure, and any potential obstructions or abnormalities, such as cysts, tumors, or kidney stones.
Nephrostomy Tube Placement: A procedure to insert a tube into the kidney to drain urine when there is an obstruction in the urinary tract, such as a kidney stone, tumor, or scar tissue. The tube allows urine to bypass the blockage and exit the body.
Ureteral Stent Placement: A procedure where a stent (a thin tube) is placed in the ureter (the tube connecting the kidney to the bladder) to keep it open when it is obstructed by stones, tumors, or scar tissue. This helps ensure proper urine flow.
Paracentesis (for fluid overload): A procedure to remove excess fluid from the abdominal cavity in patients with kidney disease who are experiencing fluid overload. The fluid is drained using a needle or catheter inserted into the abdomen.
Lithotripsy: A procedure to break down kidney stones into smaller pieces using sound waves (extracorporeal shock wave lithotripsy, or ESWL), making it easier for them to pass through the urinary tract.
Immunosuppressive Therapy Management: In patients who have undergone kidney transplantation or are suffering from autoimmune conditions affecting the kidneys, nephrologists manage medications that suppress the immune system to prevent rejection or further kidney damage.
Continuous Ambulatory Peritoneal Dialysis (CAPD): A form of peritoneal dialysis that is performed manually, where patients fill their abdomen with dialysate and drain it several times a day. This allows for dialysis without the need for a machine.
Continuous Cycling Peritoneal Dialysis (CCPD): Another form of peritoneal dialysis, but this one is performed using a machine (cycler) that fills and drains the abdominal cavity with dialysate while the patient sleeps at night.
Hemofiltration: Similar to dialysis, this procedure filters the blood in patients with kidney failure but uses a different filtration method. It is commonly used for patients in the ICU who need continuous therapy for acute kidney injury.
Blood Pressure Management in CKD: Nephrologists play a key role in managing blood pressure, particularly in patients with CKD. Procedures include 24-hour ambulatory blood pressure monitoring and the adjustment of antihypertensive medications.
Our Focused Specialties
Multi-Specialty Care Hub
Discover India’s diverse multi-specialty health departments and treatments. We’re dedicated to ensuring a healthier tomorrow, navigating the dynamic realm of Indian healthcare. Our wide range of specialties includes top-notch hospitals, selected based on quality and healthcare facilities. Join us for a personalized journey to optimal health and wellness.
Gastro-intestine
Pulmonology
Ophthalmology

Gynaecology
Nephrology
Cardiac
Hematology
Neurology

Bone & Joint
Looking for an expert !
Our Healthcare is home to some of the eminent doctors in the world

Dr Rajesh Sharma

Dr Sandeep Vaishya

Dr Sandeep Vaishya

Dr Rajesh Sharma

Dr Rajesh Sharma

Dr Sandeep Vaishya
Easy Access Links
- International Patients
- We & Why
- Core Specialites
- Common Procedures
- Hospitals
- Doctors
- Treatment Locations
- Way To Healing
- Wise to ask before
- Comfort and Satisfaction
